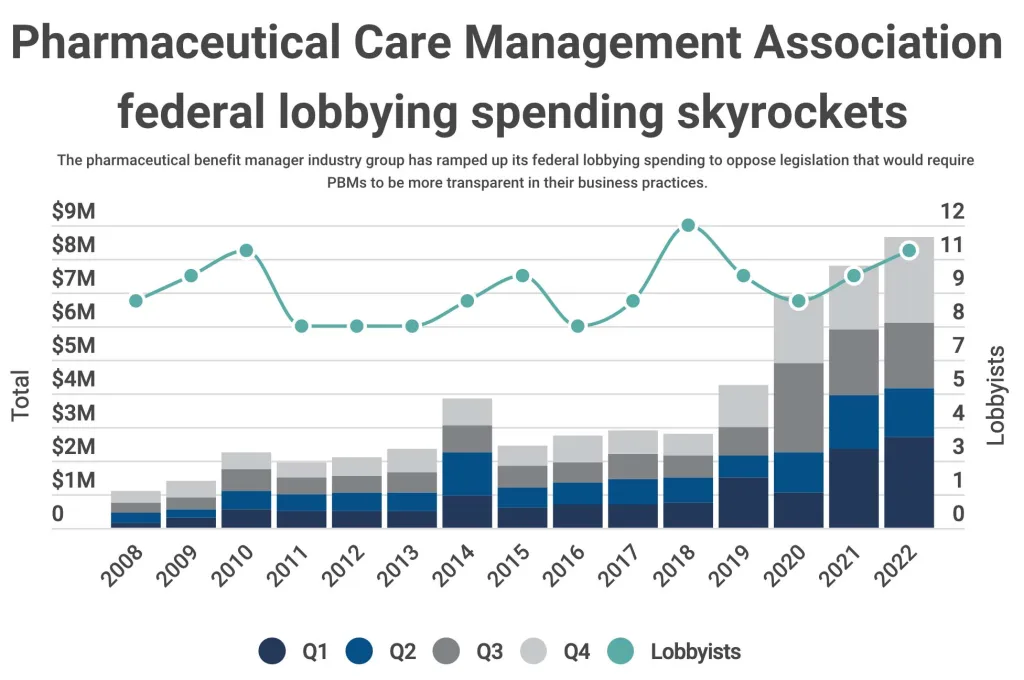
Pharmacy benefit managers, the middlemen of the U.S. pharmaceutical supply chain, are under the microscope for their role in the high price of prescription drugs. The Pharmaceutical Care Management Association, a pharmacy benefit manager trade association, has sharply increased its federal lobbying spending to oppose legislation that would require managers to be more transparent in their business practices.
Three players dominate the landscape: CVS Caremark, Express Scripts and OptumRX. Through rapid industry consolidation, these three pharmacy benefit managers controlled roughly 80% of the market. CVS Caremark, Express Scripts and OptumRX are subsidiaries of CVS, Cigna and UnitedHealth, respectively.
Pharmacy benefit managers are primarily responsible for processing and paying prescription drug claims. These third-party administrators also negotiate drug prices with manufacturers, pharmacies and insurers. Some critics argue consolidation has led to reduced competition, contributing to higher drug prices.
But the Pharmaceutical Care Management Association told POLITICO that the industry is misunderstood. J.C. Scott, president and CEO of the trade association, said pharmacy benefit managers have complex roles in the pharmaceutical ecosystem. Scott said his members—including the three biggest pharmacy benefit managers—“have a proven track record of reducing prescription drug costs in federal programs, ultimately for patients and taxpayers.”
The Pharmaceutical Care and Management Association spent $8.7 million on federal lobbying in 2022. Lobbyists for the trade association homed in on drug pricing provisions in the Inflation Reduction Act, which lowered prescription drug costs for people with Medicare, among other measures.
Eight of the 11 lobbyists registered on behalf of the Pharmaceutical Care and Management Association in 2022 previously held jobs in the federal government. One registered lobbyist, chief policy and external affairs officer Kristin Bass, was the health policy adviser to Sen. Chuck Grassley (R-Iowa) on the Senate Finance Committee in 2007 and 2008.
Grassley and Sen. Maria Cantwell (D-Wash.), ranking member and chair of the Senate Judiciary Committee, co-sponsored the Pharmacy Benefit Manager Transparency Act of 2022, introduced in the 117th Congress. The bill—another top target for the Pharmaceutical Care and Management Association lobbyists in 2022—would have empowered the Federal Trade Commission to hold pharmacy benefit managers accountable for business practices including price spreading, when a pharmacy benefit manager charges a health insurance plan more for a drug than it reimburses a pharmacy.
“The legislation is designed to award pharmacies and drug manufacturers and increase their bottom lines,” a statement from the Pharmaceutical Care and Management Association alleges. The trade association also characterized the oversight authority given to the FTC as “an egregious and unprecedented expansion of power, authority, and jurisdiction.”
The bill ultimately failed. But Grassley and Cantwell reintroduced the legislation in the 118th Congress, and the Senate Judiciary Committee passed it last Wednesday largely along party lines. The Pharmaceutical Care and Management Association continues to oppose it.
The Pharmaceutical Care and Management Association does support a pack of five bills advanced by the Senate Judiciary Committee in February. The bills include provisions that would punish the ways drugmakers keep generic and biosimilar drugs from making it to market.
One bill, the Affordable Prescriptions for Patients Act of 2023, would empower the FTC to crack down on product hopping in the pharmaceutical industry. Essentially, a company winds down production of an old drug formula then persuades or forces patients to switch prescriptions to a new drug formula. Such a switch can disadvantage generic drugs, and thus the pharmacy benefit managers that negotiate on these generic drug prices.
“The advancement of these bills will help to further limit common and egregious anti-competitive practices used to unfairly extend monopolies, and encourage greater competition and investment in more affordable options, like biosimilars, for patients,” the Pharmaceutical Care and Management Association said in a written statement.
Efforts to sway lawmakers goes beyond traditional lobbying. In 2021, the Pharmaceutical Care and Management Association sponsored a profile in POLITICO entitled “Ways Pharmacy Benefit Managers Improve Patient Outcomes,” including by encouraging competition. The trade association also recently launched an ad campaign characterizing pharmacy benefit managers as “your advocates battling the rising price of prescription drugs.”
“Advocates” or “Modern Gangsters”?
The Senate Finance Committee held a hearing Thursday morning on the impact these pharmaceutical middlemen have on the health system. Sen. Ron Wyden (D-Ore.), who chairs the committee, has been critical of pharmacy benefit managers and their impact on drug pricing.
Wyden took aim at the “perverse incentives” baked into the business practices of pharmacy benefit managers during the hearing Thursday. The chair criticized administrative fees pharmacy benefit managers charge to drug makers, calculated as a percentage of the total cost of the drug, which he said incentivizes pharmacy benefit managers to favor a similar drug that costs more.
“I believe this is an industry that is going in the wrong direction, and that’s having a big impact on the prices that Americans pay at pharmacy counters from one end of the country to another,” Wyden said in his opening statement. ”What we’re gonna have to do is look at pharmacy benefit managers with a thorough eye and take any legislative steps necessary to ensure taxpayers and patients aren’t getting a raw deal.”
In 2019, Wyden introduced the Creating Transparency to Have Drug Rebates Unlocked (C-THRU) Act. The bill, which ultimately died in committee, aimed to increase transparency in pharmacy benefit manager pricing practices by requiring pharmacy benefit managers to disclose information about their rebates and fees.
But Dr. Lawton R. Burns, professor of management and strategy at the University of Pennsylvania Wharton School of Business, told the Senate Finance Committee that pharmacy benefit managers “take the rap but get spanked for the wrongdoing of others.”
“One thing that should alleviate some concerns here is that their business models have been changing over the last five to 10 years. They no longer rely on rebates the way they used to,” Burns said. “You ought to know that manufacturers don’t like intermediaries like PBMs, very few people like intermediaries like PBMs, and that’s because they’re using leverage to extract price concessions from everyone.”
“Testimony heard today in the Senate Finance Committee largely ignored the reality that drug companies set the prices of the products they make and sell—not the companies negotiating for discounts for patients, employers and taxpayers,” Greg Lopes, assistant vice president of strategic communication at the Pharmaceutical Care Management Association told OpenSecrets in a written statement.
“Members of the committee should not be derailed by drug companies actively trying to shift attention away from the prices of drugs and the solutions on the table to reign in abuses of pricing power and patents,” Lopes wrote.
Congress, federal regulators and state officials are looking into the pricing practices of pharmacy benefit managers to assess whether any regulatory or legislative actions are necessary to address concerns about the impact on drug pricing.
Republican Ohio Attorney General David Yost filed a lawsuit against Express Scripts, Prime Therapeutics, Ascent, Humana Pharmacy Solutions and two parent companies on Monday. Yost claims the companies colluded to control drug prices, calling them “modern gangsters.”
“With this [industry] dominance, they have created a black box that holds a complex administrative system that allows the PBMs, including Express Scripts, to enrich themselves in multiple ways,” the lawsuit alleges.
The attorney general also says the pharmacy benefit managers did not live up to their promises, failing to negotiate lower drug prices and savings for patients.
The FTC is already studying the business practices of pharmacy benefit managers and their impact on patients, pharmacies and doctors. Department of Health and Human Services Secretary Xavier Becerra also addressed bipartisan concerns on the Hill last week.
“There is a growing concern that the middlemen … are skimming off a good deal of the money,” Becerra said. “We’re going to try to move to make sure that if there’s a middleman … that it’s done efficiently.”
Republished with permission from OpenSecrets, by Taylor Giorno

OpenSecrets
OpenSecrets is the nation's premier research group tracking money in U.S. politics and its effect on elections and public policy. Our mission is to track the flow of money in American politics and provide the data and analysis to strengthen democracy. Our vision is for Americans to use this knowledge to create a more vibrant, representative and accountable democracy.